African Research Journal of Education and Social Sciences, 5(1), 2018
Authors:
Emma Nordlund, DDS, Department of Dental Medicine, Division of Periodontology, Karolinska Institutet.
Tove Zander, DDS, Department of Dental Medicine, Division of Periodontology, Karolinska Institutet
Mesfin Tessma, MD, MPH, Medical Statistics Unit, Learning, Informatics Management and Ethics (LIME), Karolinska Institutet
Patricia De Palma, DDS, PhD, DDS, Department of Dental Medicine, Division of Periodontology, Karolinska Institutet
Direct correspondence and requests for reprints to: Patricia De Palma, Department of Dental Medicine, Division of Periodontology, Karolinska Institutet, P.O Box 4064, SE-14104 Huddinge, Sweden. Tel+46 8 524 881 29, Fax +46 8 711 8343. E-mail: patriciaDe.Palma@ki.se
Abstract:
To mitigate the growing migration of health care personnel from rural areas, the faculty of medicine at Makerere University changed the curriculum in 2003 and introduced Community-based Education and Service (COBES). The aim of this study was to explore how dental students perceived Community based Education and Service. Focus Group Discussions were performed at Makerere College of Health Sciences. The study employed a case study design. The participants were fourth year dental students who were involved in COBES as part of their undergraduate dental education. Focus Group Discussion method was used to collected data. The collected data were analyzed using qualitative data analysis with a focus on the manifest content of the verbal communication. Three main themes were identified, including: the students’ experience of COBES, choice of career and the future. COBES seems to improve the participants’ willingness to work in rural areas. Economy in the form of salary and good working conditions are expressed as important factors for students’ future choice of career. The study provides a glimpse of the problem and calls for a need to improve the quality of dental education and service in the COBES program. In future, studies including tutors and supervisors in higher institutions of learning can be conducted to get further information about the COBES program.
Keywords: Community-based Education and Service, Students perceptions of COBES, Attitude towards COBES, Dental students views towards COBES
1. Introduction
In Uganda the Ministry of Health (MoH) is responsible for the financing of oral health services. Only 9% of the total GDP (Gross Domestic Product) is allocated towards health service and out of this less than 0.1% is earmarked for oral health care. In health units provided by the government there is free basic oral care but patients are often compelled to look for dental care elsewhere due to lack of dental professionals, equipment and material.1
During 2007 Uganda was said to be unique since they were training two orientations of oral health workers; dental surgeons and public health dental officers. In 2006 a total of 72 dental surgeons were distributed all over the country giving 1 dental surgeon per 158 000 people. Out of these 72 dental surgeons, 39% were based in the capital city, Kampala.1
To mitigate the growing migration of health care personnel from rural areas,2 the faculty of medicine at Makerere University changed the curriculum in 2003. The traditional curriculum that was adopted in 1924, was replaced in favor of a problem-based learning [PBL] system and COBES, 3. COBES is designed in order to introduce medical students early to communities with different health needs and inspire them to work in any community despite cultural and socio-economic disparities.4 They are sent to rural areas to assess, design and implement a community project.5
Community-based learning has been reported to give students an comprehensive introduction to working in practice and give them confidence to perform both clinical and non-clinical tasks.6-8 COBES is designed to make the students aware of health problems in rural areas and to experience how life is as a rural health professional. This deliberate exposure is planned to inspire the students to consider working in a rural area of Uganda.8-10 Coming from a rural background prior to a medical education has been shown to have a stronger, positive influence on the willingness of students to work in rural areas instead of urban.11-14 The purpose of the study was to explore the views of dental students on Community Based Education and Service with reference to Makerere College of Health Sciences in Uganda.
2. Materials and Methods
Design
A A case study research design was employed to probe dental students’ perceptions of COBES. We explored the participant’s opinions on COBES by using FGD, as we believe that the dental students’ perspectives on COBES are relevant to a successful implementation of the program. The study was approved by the Research Ethics Committee at Makerere College of Health Sciences in Uganda, IRB 2013-028.
Participants
The participants were fourth year dental students who were involved in COBES as part of their undergraduate dental education at MakCHS. Students undergo a one week orientation program at MakCHS that focuses on key aspects of community- based health education. Then they are sent to community-based sites, where they spend about 4–6 weeks at a time. Purposive sampling was used to obtain a diverse sample of participants to suit the aim of the study. The inclusion criteria were that the participant had undergone their education for a few years and participated in more than one part of COBES.
Data collection
A questionnaire from an earlier study on the same topic to evaluate the opinions of students on the community-based program at MakCHS was used to develop the battery of questions 4. Two FGDs of one and a half hours each were held in English in a secluded room at Mulago Campus in June 2013. The FGDs were moderated by one of the authors, while the other author took notes at both FGDs. Participants were encouraged to express their own perceptions about COBES through an interview guide containing a predetermined set of questions that served as a checklist during the FGD. Each topic was discussed till estimated saturation. Audio recordings were made during the interviews.
Data analysis
The interviews were transcribed verbatim. The text was analyzed using qualitative content analysis with a focus on the manifest content of the verbal communication, but with openness to the latent content through interpretations for a greater understanding. Qualitative content analysis was carried out mainly according to the method of Graneheim and Lundman 2004.15 Using the method as a guide, the text was divided into units of meaning consisting of sentences and paragraphs linked together by their context in chronological order. Themes and categories were formed out of the interview guide, with the aim of investigating perceptions among the students. Then we sorted the data in categories in this early stage of the analysis to structure the information and to do an early overview of what was actually said in the interviews based on the purpose, earlier research and relevant theories.
Downe-Wamboldt’s recommendation was used in the various steps of our qualitative content analysis.16 Downe-Wamboldt (1992) recommends working with the following steps in qualitative content analysis in whatever order seems appropriate and in a process comprising pretesting followed by revision of categories and codes: 1) Selecting the units of analysis, 2) Creating and defining the categories, 3) Pretesting the category definitions and rules,4) Assessing reliability and validity, 5) Revising the coding rules if necessary, 6) Pretesting the revised category scheme, 7) Coding all the data, 8) Reassessing reliability and validity.
3. Results
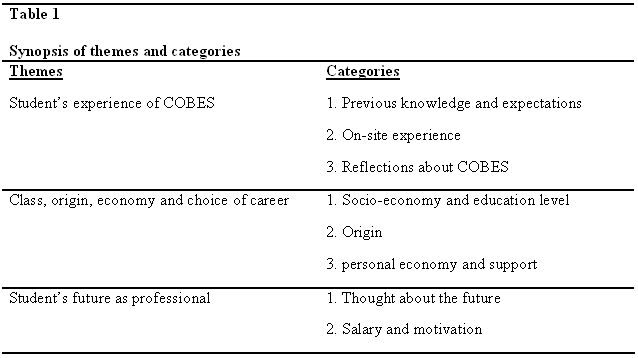
After thoroughly analyzing the materials, three major themes emerged: students’ experience of COBES, choice of career and students’ future (See Table 1).
Theme 1: Students’ Experience of COBES
Category 1: Previous Knowledge and Expectations
Students mentioned being excited going to COBES since they were anxious of what the job market would offer to them and even a significant number did not really know what to expect.
They tell you to expect culture shock. They tell you about your way of interacting with the community, and how to fit in and adopt to their cultures. You have to try as much as possible to reason with the people so as to ensure you deliver the best services. This exposure is important since would allow us students to gain the best in terms of work experience.
“[…] I expected to find a state-of-the-art hospital with a lot of personnel but when I got there I was actually surprised since there were only two doctors […]”
Category 2: On Site Experience
The students reported lack of appropriate hospital equipment, lack of medicine and poor hygiene standards at the clinics, and these poor working conditions greatly affected proper service delivery. The dental clinic sites were not properly facilitated and had no functional dental units. Most dental services were lacking and only tooth extraction services were being offered.
“[…] if they sent you to dental clinics, I realized that in most of those government hospitals where we were stationed , the only thing that is functioning in these dental units is extraction. […] so you are going to learn how to give local anesthesia and extract. That’s all […]”
“The other thing is that services, that we are used to here are syringes in plenty,”
“ At that site we actually don’t have those services and it is quite difficult to adjust […]”
They also reported lack of personnel and especially lack of educated tutors.
“ I expected to find people who are more educated, someone who can explain to you something why they are doing it and the physiology and everything behind it. But they don’t know these things because they learnt from experience. It was kind of a disappointment.”
The students’ experiences of the personnel at site were that they had very low motivation for their work and they thought it was because of their low salary and challenging working conditions.
“[…] these people know we are coming because they are told earlier and we go there every year but some of them are never prepared […] they are trying to give what they have, but in most cases most of them are not motivated”
The personnel did not seem to know about the program or the students’ presence.
“[…] usually it’s the head of the hospital and our site tutor who knows. But the rest of the hospital.. the people are just seeing you […] they don’t even introduce you!”
“Some of those people are said to be there, but they are not there. Probably they are there once in a week, but have to look for money elsewhere.”
One of the site personnel tutoring the students complained that they were not being properly compensated for the tutoring services and that it was not part of their job description, therefore the person was not paid for it.
At the respective work centers, the students’ had different experiences – some sites arranged accommodation and others did not. The students complained on inconveniences such as long distances to the work stations and high cost of food were a major challenge to the students considering the limited amount of allowances. The students however solved these challenges in different ways such as buying cheap fast-foods from local eateries, while others opted to prepare home made meals. A significant number of students were privileged enough to get free meals and accommodation from the host community.
“Accommodation was a challenge since there were very limited number of rooms and there was limited resources in terms of beddings.”
“The location I was posted to during my first year, accommodation was provided for and the host community were hospitable.”
Category 3: Reflections about COBES
Most Focused Group Discussion participants saw COBES as a good idea since it is an opportunity to meet different cultures and communities. They also stated that it exposes them to work environment in the rural setting where there are limited resources.
“I think COBES is a very effective program. But I think we as students need to embrace and appreciate it more and I think the students probably need more allowances so as to boost their working morale and cater for basic necessities.”
This program has also improved the social interaction among students from different backgrounds, where they share experiences gathered from different work backgrounds.
“… making friends. You learn a lot of stuff, it’s good. It’s good for both personal and career progress… ”
A common trend drawn from the students’ experiences was that COBES puts too much focus only on medical students. The host communities proposed that the programme be extended to cover other health concerns and not only dental services. They also proposed that a permanent centre should instead be set at respective facilities as part of COBES commitment to reach out to a large number of residents even if it is for a subsidized cost. This would have served them more efficiently.
“The whole program only focuses on dental care services”
“They should go an extra mile and start introducing other medical services in the program […] it should be broad and not only dental services, or at least set up a permanent dental clinic.”
In terms of clinical exposure before COBES, the students reported having visited hospitals but not dental clinics and therefore were a bit disappointed. Lack of proper induction process at the respective work stations contributed significantly to poor service delivery by the COBES students. Most people at these facilities were not aware of what services the students were offering.
Theme 2 Class, origin and economy
Category 1: Socio-economy and Educational Level
There was a common agreement among the students that socio-economic factors have a lot of influence on matters regarding choice of career in Uganda.
“I think it varies because most medicine students come from wealthy backgrounds and therefore can afford to enroll them in expensive medical schools.”
Category 2: Origin
Several of the participants were in agreement that despite coming from urban or rural setups, ones exposure also has a hand in the way the medical student delivers their skills at work.
“[…] people who come from rural areas they don’t really know that medical school has dental school. […] but people who have grown up in town are exposed to such services and hence enroll in bigger numbers for this course.”
Category 3: Personal Economy and Support
Some students affirm that education is expensive and that students who cannot afford the fees find it tough to study these courses that are expensive, and are forced to seek funds to enable them enroll for these courses through fundraising from family and friends, and through application of loans.
“You actually need support because without it, learning will literally be impossible and quite difficult.”
Theme 3: Student’s Future as Professionals
Category 1: Thoughts about the Future
When asked about their future as dentist professionals all students agreed that the government pay to such professionals is low, while they are forced to work for long hours which goes uncompensated. Some students mentioned that they indeed deserved better remuneration since they had invested a lot of funds in their education and the government should consider that when reviewing their salaries.
“[…] I prefer working where remuneration is better than in government. Most of us end up having debts which we accumulate from loans and from other sources that enabled us enroll in this medical courses, and that is why we consider the high salary after school so that we pay these debts and spare some money for our upkeep.”
Category 2: Salary and Motivation
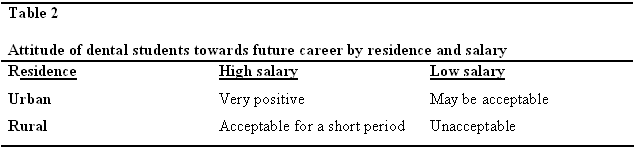
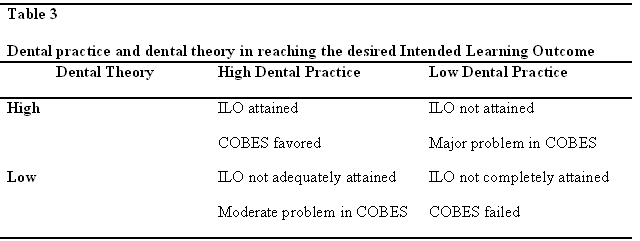
Most of the students want to give back to the community and some even feel obliged to return. Most students are for the opinion that experience from a high number of patients is more important than the salary for a start since it exposes them to work experience which boosts their skills. The reflection of the students is summarized in Tables 2 and 3.
“The main reason as to why you’re in school is to earn a better living later, to live and give back to the community, to give back to your family […]”
“Personally I would love to work at a place where I earn more and it would really encourage me to give back to the community if need be.”
“I think for a start I can work in an urban setting, since there are more allowances offered, and later on save and invest back in my rural village.”
4. Discussion
This study discusses the pros and cons related to COBES among dental students. The study has helped to bring out dental students’ perspective of COBES and has explored a range of factors which have affected students’ attitude and perceptions during their experience while working for the COBES program. The key findings show mixed attitude both (positive and negative) towards COBES. However, most students are positive about the program, but also wanted prior training concerning the program be made thorough for students to fully embrace it.
Information offered by the university was considered less detailed. Proper orientation should be done to students both at school and at the ground where the students will be based. This is important since it helps students be comfortable and learn to adopt to the different environments they will be exposed to. This will minimize the culture-shock impacts to some students.
Most students were excited to take part in COBES but over time, but the students morale kept on decreasing as they faced work challenges This might imply that there is a decreasing excitement and therefore the students felt more positive towards rural placement in the initial years. Leaving the city for placement in rural areas means constraints in clinical and educational resources, as well as living conditions.
The students had expected enthusiastic and well-informed tutors and site personnel, but seemed the tutors had not gained the necessary training skills and their understanding of the content also was put to question. Some were not aware of the student’s presence at sites. Due to this, students felt unwelcome, unprepared and invisible.
One of the predominant findings that emerged from the study was that dental students felt marginalized and felt that dental education was not treated as an equal to medical education in COBES.17
However, COBES had a positive impact at a personal level since the students in several cases had their first hands-on experience which led to increased confidence. Other participants said they felt like they had accomplished something and that the program gave them a wider spectrum of thinking. Thus, unlike medical students who have positive attitudes, dental students have a mixed attitude towards COBES.17
The opinions of how accommodation and food were organized ranged from very good to terrible. At some sites the students felt very accepted and cared for, while at others arrangements were a struggle, a feeling of being treated unfairly. This may decrease motivation and may lead to a negative attitude towards COBES. Some participants mentioned lack of motivation for COBES since the program needs more finance and better facilities to improve the experience of the program.
There is a shared agreement amongst the participants that origin and socio-economic factors influence choice of career as a dentist in Uganda. Many students originate from urban areas and the majority of the participants’ families are well-educated. In urban areas educational possibilities are known and readily available compared to rural areas. Further contributing factors here could be the economic situation of a student’s family and the expectations from well-educated families and relatives to earn a high degree at the university. Some researchers reported that students with a rural origin are more likely to show willingness to practice in rural areas.18—19 But participants stated that they have invested a lot in their education and therefore salary is quite important for them.
Working conditions were perceived as hard during their visits to COBES sites. The lack of equipment and medicine ultimately may lead to many problems including hygiene and many of the students seem to be unwilling to work in these conditions five days a week. They all want to give back to the community but consider it to be mainly about goodwill.
The concern that dental education is being omitted in favor of medical education was palpable. The students mentioned that the program in general is related to medicine and is not to a larger extent connected to their future profession. COBES needs to be connected to the students’ future career and related to the practice that they can use in their future career. If the student finds that COBES is not related to dentistry but medicine then it demotivates the person to enjoy the program. The participants requested more dental tutorial problems and desired a dental clinic, or at least a visit, at every COBES site.
5. Conclusions and Recommendation
Unlike medical students17, dental students have mixed attitudes towards COBES. It seems how dental students perceive COBES is dependent on the content and delivery of dental education, the quality of the education given, the presence of resources to conduct the program, the practical knowledge gained, the opportunity to conduct dental services and the preparation for future working life. Thus, a number of issues regarding the implementation need to be addressed in order to reach the intended educational and service goals. Education providers need to have clear processes for identifying and responding to COBES concerns during the rural attachment. Even though the scope assessed is narrow, it still provides a glimpse of the problem and calls for a need to improve the quality of dental education and service in the COBES program. The university, therefore, will need to implement appropriate measures to both minimize and ameliorate such issues. Generalization of the findings for large areas requires more elaborate surveys. In future, studies including tutors and supervisors can be conducted to get further information about the COBES program.
Owing to the limitation of time, the study was conducted only among the fourth year dental students who were involved in COBES as part of their undergraduate dental program. The study should have involved more participants from different departments and classes, tutors and supervisors. Further study could be undertaken to include more institutions of higher learning in Uganda.
Acknowledgements
We would like to express our appreciation to Annet Kutesa, Loui Muvazil and Andrew Mwanika for their contribution in organizing the research activities at Makerere University. We are also very grateful for the willingness of the students to participate in the study and Conny Abrahamsson for his support during the study. Last but not least we will express our gratitude to Chris Mortimer for his linguistic review of the manuscript.
Funding
This study was financially supported by The Department of Dental Medicine, Division of Periodontology, Karolinska Institutet, Stockholm, Sweden.
Disclosure
The authors declare that they have no conflict of interest. The study was initiated and financially supported by The Department of Dental Medicine, Division of Periodontology, Karolinska Institutet, Stockholm, Sweden.
References
- National oral health policy [Internet]. Uganda. Ministry of Health; 2007. Cited 131103. Available from: http://library.health.go.ug/publications/service-delivery-child-health/oral-health/national-oral-health-policy Page 6-7
- Recruitment of health workers from the developing world. Report by the Secretariat [Internet]. WHO 2004; Cited 121022. Available from: http://apps.who.int/gb/archive/pdf_files/EB114/B114_5-en.pdf
- Kiguli-Malwadde E. et al., Problem Based Learning, curriculum development and change process at Faculty of Medicine, Makerere University, Uganda. Afr Health Sci. 2006 June; 6(2): 127-130.
- Community Based Experience and Services: An innovative Medical Education of University of Ilorin, Nigeria [Internet]. Ilorin. College of Health Sciences; 2008-10. Cited 131111. Available from: http://www.cohs.unilorin.edu.ng/index.php/cobes/about-cobes
- Chang LW et al. Perceptions and valuation of a community-based education and service COBES program in Uganda. Medical Teacher; 2011;33(1):e9-15.
- Lynch CD., Ash PJ., Chadwick BL., Evaluation of a community-based clinical teaching programme by current and former student dental therapists and dental hygienists: a pilot investigation. Br Dent J. 2011 May 28;210(10):481-5.
- Lynch CD, Ash PJ, Chadwick BL, Hannigan A. Effect of community-based clinical teaching programs on student confidence: a view from the United kingdom. J Dent Educ. 2010 May;74(5):510-6.
- Mwanika A. et al. Perception and valuations of community-based education and service by alumni at Makerere University College of Health Sciences. BMC Int Health Hum Rights. 2011;11(Suppl 1):S5.
- Howe A. Patient-centred medicine through student-centred teaching: a student perspective on the key impacts of community- based learning in undergraduate medical education. Educ. 2001 Jul;35(7):666-72.
- Kaye D. et al. The organization and implementation of community-based education programs for health worker training institutions in Uganda. BMC Int Health Hum Rights. 2011;11(Suppl 1):S4.
- Florence JA., Goodrow B., Wachs J., Grover S., Olive KE. Rural health professions education at East Tennessee State University: survey of graduates from the first decade of the community partnership program. J Rural Health 2007 Winter;23(1):77-83
- Henry JA., Edwards BJ., Crotty B. Why do medical graduates choose rural careers? Rural Remote Health. 2009 Jan-mar;9(1):1083.
- Wilson NW et al. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural and Remote Health 9:1060, 2009; June.
- Richards HM., Farmer J., Selvaraj S. Sustaining the rural primary healthcare workforce: survey of healthcare professionals in the Scottish Highlands. Rural and Remote Health 5:365, 2005; March
- H Graneheim, B. Lundman. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004 Feb;24(2):105-12.
- Downe-Wamboldt B. Content analysis: method, applications and issues. Health Care Women Int. 1992 Jul-Sep;13(3):313-21
- Chang LW, Kaye DK, Muhwezi W, Nabirye RC, Mbalinda S, Okullo I, Groves S, Kennedy CE, Bollinger RC, Sisson S, Burnham G, Mwanika A: Perceptions and valuation of a community-based education and service (COBES) program in Uganda. Medical Teacher, 2011, Vol. 33, No. 1 , Pages e9-e15
- Laven G., Wilkinson D. Rural doctors and rural backgrounds: how strong is the evidence? A systematic review. J. Rural Health. 2003 Dec;11(6):277-84
- Easterbrook M. et al. Rural background and clinical rural rotations during medical training: effect on practice location. CMAJ. 1999 Apr 20;160(8):1159-63

